Pharmacogenetics
The pharmaceutical industry is constantly changing, and so, too, are Skilled Nursing Facility pharmacy solutions. As science discovers more about how the human body functions and metabolizes medications, the potential to personally optimize medications for patients increases.
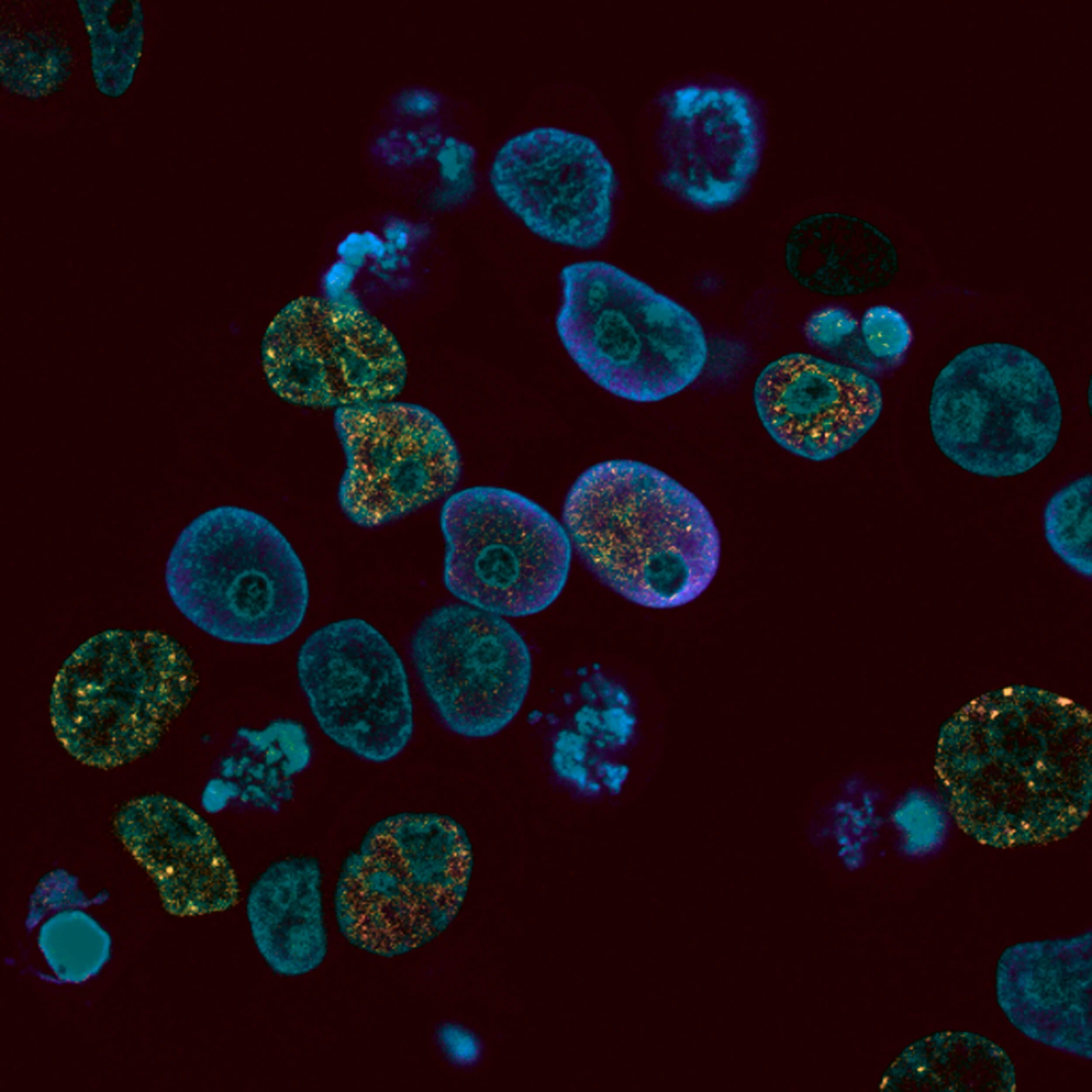
The topic of pharmacogenetics is increasing in popularity as we progress towards personalized medicine. We have learned a significant amount about how an individual’s genetic makeup impacts how medications are metabolized, which affects the efficacy and safety of a medication.
The missing link in most situations is understanding each patient’s genetic makeup so that can be related to the therapies he or she receives or may receive in the future.
Cost saving of incorporating PGx in LTC:
Rising medication costs are a significant concern nationwide and in skilled nursing. Today, prescription drug expenditures account for nearly 20 percent of healthcare costs, and prescription spending is growing faster than any other part of healthcare.
-
American spending on prescription drugs increased 13.1 percent in 2014—the largest annual increase since 2003.
This uptick was largely driven by an unprecedented 30.9 percent increase in spending on specialty medications. In 2015, spending rose another 12.2 percent.
Specialty drug pricing alone is far outpacing the Consumer Price Index, and specialty drugs increased to 44 percent of overall drug spending in 2017.
Prescription spending in long-term care is approaching the $17 billion level with nearly 400 million prescriptions dispensed in 2016.
The Potential of Pharmacogenetics
Pharmacogenetics holds the potential of providing medical practitioners with specific genetic data that will allow us to tailor medications to individual patients. Providers could predict dangerous adverse reactions or identify therapies that would not be effective for individual patients if they could know a patient’s genetic makeup.
Routine pharmacogenetics is not normal practice at this time, but there are specific situations when it may benefit in current situations, including with anticoagulation and antiplatelet therapy.
Adverse drug events and medication nonadherence are a leading cause of hospitalization among patients. The majority of emergency hospitalizations caused by medication issues are linked to five specific types of medications: warfarin, insulin, oral antiplatelets, diabetic medications, and opioid pain medications.
In our efforts to reduce unnecessary hospitalizations, we must be willing to investigate newer, challenging avenues to find the root cause of medication-related issues & outcomes.
Pharmacogenetics and Anticoagulant Therapy
Clopidogrel, otherwise known as the brand Plavix®, is a popular antiplatelet medication in long-term care pharmacy. Pharmacogenetics is a pertinent topic related to clopidogrel because clopidogrel is a prodrug, a type of medication that must be metabolized through the cytochrome P450 system before it becomes an active medication.
If a resident’s cytochrome P450 enzyme system is not functioning at its expected level, this will result in metabolism variations when processing clopidogrel, which ultimately means the medication may not be metabolized to the necessary active form. Basically, we could be administering the medication to a resident exactly as ordered, but the body may not be reacting to it the way we expect. Pharmacogenetics would allow us to know if a resident’s cytochrome P450 system is functioning as expected prior to prescribing the medication. Warfarin, popularly known as Coumadin®, is another key example.
Warfarin has a number of potential interactions with both foods and other medications. In addition, warfarin can also be very difficult to stabilize in some residents. The difficulty in stabilization could be caused by two different situations.
First, warfarin is metabolized significantly by the cytochrome P450 system, so variations in a resident’s cytochrome P450 system detected through pharmacogenetics could affect the plasma levels and processing of warfarin in the body.
Warfarin is also unique because of the VKORC1 enzyme, which controls the oxidation state of vitamin K. VKORC1 normally works to activate vitamin K as part of the normal process of blood clotting. Warfarin inhibits VKORC1, which reduces vitamin K oxidation and reduces clotting.
If a resident has lower levels of VKORC1, less warfarin will be needed to impact clotting. If this is not known and a resident receives a standard dose of warfarin, he or she may experience an increased risk of side effects, such as bruising and bleeding.
If pharmacogenetics were used, healthcare professionals would have cytochrome P450 and VKORC1 genetic information available to them when prescribing medications. This would allow for more appropriate doses of medication for the resident, tailored to his or her bodily processes, for more optimal results.
Pharmacogenetics and the Future
Once a pharmacogenetics test has been completed, it does not need to be repeated. The resulting data can be applied to the resident’s entire therapeutic regimen and taken into consideration before any future prescriptions to make his or her medication regimen specific and personalized.
Healthcare providers routinely encounter situations where things don’t work out as expected, or simply can’t be reconciled with medical training or experience. This is because of our unique human body, and factors we cannot detect.
Medical care of the future, armed with pharmacogenetics, will provide all that is needed to make optimal medication decisions for residents.
Participants, family members, and providers in the PACE environment should all be familiar with medications and medical conditions that increase the risk of falls. Medications—and their side effects—are one of the major causes of falls in the elderly. Because of the potential for injury when an older person falls, everyone in the PACE environment should be aware of which medications or conditions come with an increased risk of falls. When it’s possible, providers should seek safer alternative medications or even reduce medications to the lowest effective dose as a fall prevention strategy.
Medication Criteria in the PACE Environment
For more than 20 years, the American Geriatrics Society has provided a continuously updated resource for providers to improve the safety of older adults who take medications. The BEERS Criteria for Potentially Inappropriate Medication is the gold standard for prescribing safe medications for older adults in the PACE environment. As PACE participants grow older, their bodies change. Because of these body changes, older adults have a higher risk of unintended or exaggerated side effects from their medications. Each year, one out of three seniors aged 65 or older encounters at least one adverse medication reaction. While the BEERS Criteria is a valuable tool, it cannot be the only guide when prescribing medications for participants in the PACE environment. Different participants respond differently to the same medications. Experienced clinical judgement must be included in every prescription choice.
Anticholinergic Medications in the PACE Environment
Anticholinergic medications inhibit certain nerve impulses, thereby reducing spasms of smooth muscles like those found in the bladder. These drugs are used commonly among senior adults in the PACE environment. Some medications, such as atropine, benztropine, and oxybutynin, are used specifically for their anticholinergic properties, and others such as diphenhydramine, cyclobenzaprine, and olanzapine have anticholinergic properties unrelated to their primary use. Studies have shown that medications with anticholinergic properties can have adverse side effects like blurred vision, dry mouth, urinary retention, constipation, cognitive impairment, confusion, delirium, increased heart rate, and drowsiness. These conditions can significantly increase the risk of falls. The risk of falls increases when taking medications with strong anticholinergic properties, taking higher doses of these medications, or taking a combination of them. Adults in the PACE environment are also more likely to experience adverse events from anticholinergic medications because of bodily changes and preexisting conditions. When possible, medications with anticholinergic properties should be avoided in older adults unless they are absolutely necessary. If the medication is necessary, it should be used at the lowest dose for the shortest possible time. Providers in the PACE environment should also consider replacing such medications with alternatives, including non-medicinal solutions.
Falls in the PACE Environment
It may be impossible to eliminate falls altogether, but everyone should be concerned with reducing the risk of falls throughout the PACE environment. When a fall occurs, it is vital to evaluate the participant’s medications and determine what may have contributed to the fall. For example, if a participant recently suffered a fall, look through recent records and see if a medication dose has been increased, a new medication has been added, or if the participant has been requesting more of a medication that could contribute to a fall. By constantly reviewing each participant’s therapies, talking with family members, and creating action plans when a fall occurs, everyone concerned with the PACE environment can provide participants with the best care possible.